Ophthalmology is one of the topics to understand for the USMLE Step 3, ABIM, and on other medical exams where internal medicine is a major focus. The following is an excerpt out ofCracking the USMLE Step 3.
Exclusive visual from the Knowmedge QVault
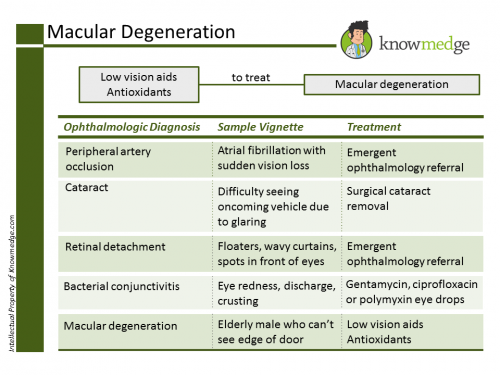
- Painless loss of central vision
- See drusen (i.e., yellow deposits) in the macula on ophthalmoscopic exam
- Treatment is low-vision aids, antioxidants and sometimes laser photocoagulation to delay loss of vision in exudative macular disease
- Acute onset -Typical history is person sitting watching a movie in dark theater with sudden blurry vision that is usually unilateral
- Signs and symptoms include:
- Tender, hard eye
- Red eye
- Dilated pupil that is semi-responsive to light
- Obtain stat ophthalmologic consult
- Conduct tonometry (i.e., measure pressure in the eye) for diagnosis
- Treat with IV acetazolamide or acetazolamide eye drops
- Carbonic anhydrase inhibitors – decrease the production of bicarbonate
- Can also give β blocker eye drops (i.e., timolol)
- Consider cholinergic eye drops (i.e., pilocarpine)
- Never give anticholinergics to patients with glaucoma
- Definitive treatment is laser iridotomy
- Occurs more gradually as vision is lost
- Painless
- Treatment is to decrease intraocular pressure with topical eye drops (i.e., acetazolamide, timolol, or pilocarpine)
- Never give anticholinergics
- Definitive treatment is laser iridotomy
- Clouding of the lens
- Patients may present with loss of visual acuity
- Requires ophthalmologic follow-up with slit-lamp examination
- Treatment is usually surgical if vision loss is progressive and discomforting
- Difficulty for lens to focus
- Decrease in near-sightedness
- Presbyacusis – loss of hearing with age (i.e., usually high frequency sounds)
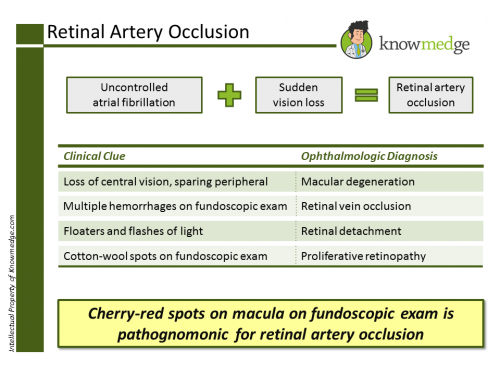
Central Retinal Artery Occlusion
Exclusive visual from the Knowmedge QVault
- May be from emboli
- May be from atherosclerosis or Diabetes
- Sudden blurry vision or loss of vision in one eye
- Painless -May respond poorly to light, but will constrict abruptly when light shined in other eye
- See cherry red spot on the macula and a pale fundus
- Treat with thrombolysis if within 8 hours since symptom onset
- Consider IV acetazolamide or timolol to decrease intraocular pressure
- Prescribe aspirin daily
- If suspect may be secondary to temporal arteritis, start IV prednisolone immediately and schedule temporal artery biopsy
- Visual loss is painless and occurs gradually
- Ophthalmologic exam is critical
- Dilated tortuous veins
- Retinal hemorrhages
- Cotton-wool spots
- Macular edema
- Treat with laser photocoagulation
- Especially for diabetic retinopathy with neovascularization and branch retinal vein occlusion
- Prescribe aspirin daily
Exclusive visual from the Knowmedge QVault
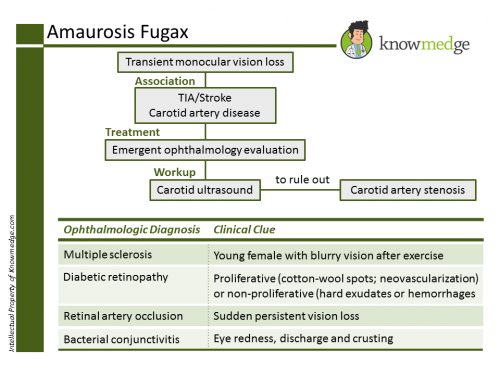
- Sudden, transient loss of vision
- Usually unilateral
- Described as a curtain coming down vertically over the visual field
- Caused by transient ophthalmic artery (i.e., branch off internal carotid artery) occlusion
- Ultrasound carotids to detect degree of stenosis
- If greater than 70 % stenosis with symptoms (i.e., amaurosis fugax), carotid endarterectomy is indicated
- May also do Stenting or balloon angioplasty
- If carotid stenosis greater than 60 % and patient asymptomatic, carotid endarterectomy indicated
- Prescribe aspirin daily
- Lesion of Right Optic Nerve
- Blindness in right eye
- No reaction to light in right eye
- Left eye does not constrict with light in right eye
- Lesion at Optic Chiasm
- Patients present with bitemporal hemianopsia
- Seen in pituitary tumors, craniopharyngiomas, or Rathke’s cleft cyst
- Lesion of Right Optic Tract
- Causes a contralateral homonymous hemianopsia with loss of macular vision
- Lesion of Right Optic Tract in Meyer’s Loop in Temporal Lobe
- Causes a left superior quadrantonopsia (i.e., “pie in the sky”)
- Lesion of Right Optic Tract in Parietal Loop in Parietal Lobe
- Causes a left inferior quadrantonopsia
- Lesion in Right Occipital Lobe
- Causes a left homonymous hemianopsia with macular sparing Seen in posterior cerebral artery (PCA) distribution infarctions
- Autosomal recessive
- Mutation of RB1 gene(Tyrosine kinase)
- Mutation on chromosome 13
- Most distinctive sign is leukocoria
- White spot present in the patient’s pupil upon light testing
- If detected on ophthalmoscopic exam, treatment is stat ophthalmology consult
- Treatment is enucleation
This post was originally posted on the Knowmedge Blog.
No comments:
Post a Comment